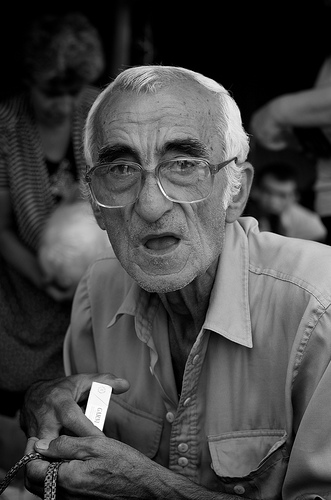
Are you worried that an elderly loved one has been a victim of financial abuse? Each day, older adults become targets for financial scammers. Commentators are concerned that privacy laws are likely to protect some of these financial scammers, preventing elderly victims from seeking justice. According to Herb Weisbaum, “The Consumer Man” for NBC News, there’s a major disconnect in the financial world. “When,” he asks, “does the suspicion that an elderly customer is being defrauded overcome laws protecting privacy rights?” In an earlier post, we mentioned that banks might be “quiet enablers” of this kind of elder abuse.
The problem of elderly financial abuse occurs across the country, and California isn’t immune. Who is responsible for making sure that older adults aren’t taken advantage of financially? For many victims of elder financial abuse, the ramifications are just as vicious as physical nursing home abuse. If you suspect that your elderly parent or loved one has been the victim of a financial crime, it is important to contact an experienced elder justice advocate. With years of experience handling nursing home abuse and neglect cases in Southern California, the dedicated elder law attorneys at the Walton Law Firm can speak to you today about your claim.
Bank Employees in a Position to Help?
 California Nursing Home Abuse Lawyer Blog
California Nursing Home Abuse Lawyer Blog


 This news is only the latest in many reports concerning elderly dementia patients and the varied problems of antipsychotic drugs. Indeed, the California Department of Public Health and the Department of Health Care Services have been working to reduce the “off-label” use of
This news is only the latest in many reports concerning elderly dementia patients and the varied problems of antipsychotic drugs. Indeed, the California Department of Public Health and the Department of Health Care Services have been working to reduce the “off-label” use of  Many states have been tightening their oversight of home care agencies over the past several years, due to a general sense of inadequacy in the services provided by these companies. And now, California has joined that group. According to an article in the New York Times, “California has become the latest state to tighten oversight of home agencies that provide custodial care—help with bathing, dressing, toileting and other basic tasks—to older adults and people with disabilities.”
Many states have been tightening their oversight of home care agencies over the past several years, due to a general sense of inadequacy in the services provided by these companies. And now, California has joined that group. According to an article in the New York Times, “California has become the latest state to tighten oversight of home agencies that provide custodial care—help with bathing, dressing, toileting and other basic tasks—to older adults and people with disabilities.” While many assisted living facilities in California may be providing appropriate care and abiding by the law, many of these homes continue to expose their residents to serious cases of abuse and neglect. If you have an elderly loved one who resides in a nursing facility, it’s important to make sure that your loved one receives the best care possible. If you’re concerned about nursing home abuse or neglect, don’t hesitate to contact an
While many assisted living facilities in California may be providing appropriate care and abiding by the law, many of these homes continue to expose their residents to serious cases of abuse and neglect. If you have an elderly loved one who resides in a nursing facility, it’s important to make sure that your loved one receives the best care possible. If you’re concerned about nursing home abuse or neglect, don’t hesitate to contact an  Are you concerned about the kind of care your elderly loved one currently receives? No one should have to worry about
Are you concerned about the kind of care your elderly loved one currently receives? No one should have to worry about  Limited Dental Care Training and Attention
Limited Dental Care Training and Attention Details of the Documentary Series
Details of the Documentary Series Older Adults Don’t Anticipate Nursing Care
Older Adults Don’t Anticipate Nursing Care